Community Resource Initiative’s clinical research helps find safer, more effective, and more convenient ways to treat HIV and other infectious diseases.
Our trials enable research participants to be more active in their own healthcare, to gain access to new treatments before they become widely available, and to help others by contributing to ground-breaking medical knowledge.
If you have questions about Community Resource Initiative’s clinical trials or would like more information about currently enrolling clinical trials, click here or contact the Community Resource Initiative Research Team.
Contact the Research TeamOngoing and Recent Clinical Trials

DEFINE
Closed
The DEFINE clinical research study measures changes in weight and body composition after switching HIV treatment to a single tablet regimen, Symtuza, which is FDA approved for adults living with HIV-1.
Define Clinical Trial
Islatravir in Combination with Lenacapavir
Ongoing (no longer enrolling)
Study Evaluating the Safety and Efficacy of Islatravir in Combination With Lenacapavir in Virologically Suppressed People With HIV.
A Phase 2 Randomized, Open-Label, Active-Controlled Study Evaluating the Safety and Efficacy of an Oral Weekly Regimen of Islatravir in Combination With Lenacapavir in Virologically Suppressed People With HIV.

Islatravir in Combination with Doravirine
Ongoing (no longer enrolling)
A Phase 3, Randomized, Active-Controlled, Double-Blind Clinical Study to Evaluate a Switch to Doravirine/Islatravir. Once-Daily in Participants With HIV-1 Who Are Virologically Suppressed on Biktarvy.
Learn more about this trialPast Clinical Trials
The START (Strategic Timing of Antiretroviral Treatment) Study, a large-scale clinical trial for which CRI was one of hundreds of international research sites, found that people with HIV should start antiretroviral (ARV) therapy as soon as possible after diagnosis to avoid developing AIDS and opportunistic infections. The START study showed that participants who began ARV treatment immediately after diagnosis were 53 percent less likely to die during the trial, develop AIDS, or develop another serious illness, compared to those who waited to begin ARV treatment. These data are the collective effort of staff at research sites around the world, and most importantly, the 4,685 participants who volunteered to be followed for multiple years to help definitively answer the question of when to start ARV treatment.
The START Study findings were so robust that they influenced international guidelines on HIV treatment. Previously, the World Health Organization’s (WHO) guidelines said a patient should wait until his or her CD4 level had fallen under 500 to begin treatment. Both the WHO and the U.S. Department of Health and Human Services have updated their guidelines to advocate for starting treatment as soon as possible after diagnosis.
An estimated twenty-five percent of individuals infected with HIV in the U.S. are also infected with the Hepatitis C virus (HCV), an infectious disease of the liver. Left untreated, HCV can lead to liver failure, liver cancer, and premature death. Co-infection with HIV significantly increases these risks. Until just recently, individuals undergoing treatment for HCV faced the same terrifying uncertainty as those with HIV in the 1980s and early 1990s.
“Participating in the ION hepatitis C (HCV) trials was another significant landmark for us at CRI,” said Former CRI Associate Research Director and Principal Investigator Dr. Hannah Bouldin Olivet. “One of these trials showed that a single-tablet, two-drug, non-interferon regimen for HCV was not only possible, but could cure a particular population at least 98% of the time. Offering this kind of a trial for people co-infected with HCV and HIV—our second ION trial—was also a game-changer, because the cure rates were equally as impressive for them.” These trials prompted the approval and broad availability of the first drug in a new generation of well-tolerated and safe curative treatments for hepatitis C.
In 2005, a pilot study initiated and conducted by Community Research Initiative investigators suggested a novel short-cycle intermittent treatment approach for HIV might be an effective way to sharply cut the cost of treating the disease and enhance the quality of life of patients facing decades of powerful and sometimes toxic drug exposure periodically accompanied by devastating side effects.
CRI researchers theorized that medication levels might not be significantly affected by a two-day break from select antivirals that have a prolonged half-life in the body, assuring that the virus would remain in check. Tests showed after 48 weeks on the FOTO (Five Days On, Two Days Off) study, patients on efavirenz-based antiretroviral therapy maintained a high rate of virus suppression.
To follow up on the positive results of this proof of concept study, a multi-site pilot study was conducted. Sixty subjects, all on daily efavirenz/tenofovir/emtricitabine (EFV/TDF/FTC) with CD4 count>200 and durable viral suppression, were randomized to continue daily therapy or change their weekly schedule to five consecutive days on treatment (typically Monday–Friday) followed by two days off treatment (five on, two off, or “FOTO” schedule). The larger pilot study confirmed the smaller study’s original results and showed that all participants on the FOTO regimen maintained virologic suppression through 48 weeks of treatment and expressed a strong preference for the FOTO schedule.
Researchers and patients around the world continue to express interest in short cycle therapy with antivirals. A similar study conducted in Europe, Africa and Asia (BREATHER study) replicated the FOTO study findings in an adolescent population, where virologic suppression rates and patient satisfaction were high in the short cycle therapy cohort.
This study examined the safety and effectiveness of switching to long-acting cabotegravir (CAB LA) and long-acting rilpivirine (RPV LA) administered every eight weeks compared to CAB LA + RPV LA administered every four weeks (Q4W) over a 48-week treatment period in approximately 1,020 adult HIV-1 infected subjects. Participants receive injections of the medication every four or eight weeks onsite at AccessHealth MA’s research facility in Boston.
Meet our Research Team
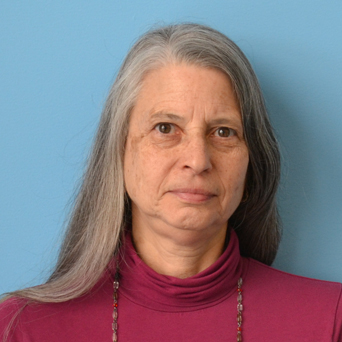
Roberta Bauer
Regulatory Specialist, Data Manager

Karen A. McLaughlin, CCRC
Research Senior Manager

David Huckle
BRIDGE Team Health Insurance Enrollment Specialist and Research Associate
